There are more than 200 diseases called cancer and they all start when abnormal cells in a part of the body divide uncontrollably, growing with reckless abandon. Why these bad cells run amok is the focus of thousands of researchers across the world and billions of dollars.
The current consensus among the vast majority of researchers is that most if not all cancers are caused by a change in or damage to genes, collectively called “mutations.” But research from two Georgia Institute of Technology cancer geneticists may alter the prevailing view.
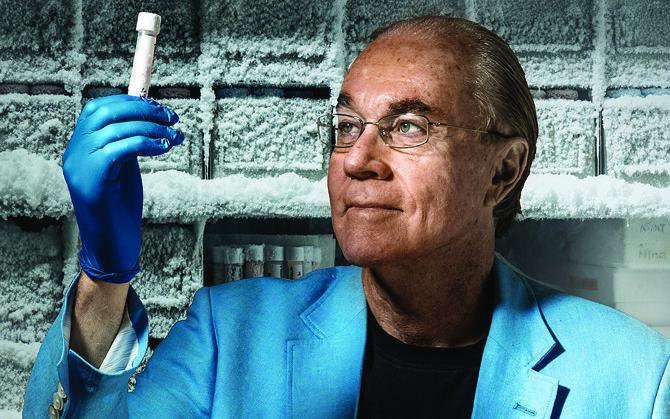
“With the exception of the few things that we know are related to predisposition, the consensus view now is that cancer is due to ‘de novo’ mutations,” says John McDonald, professor of Biology and director of the Integrated Cancer Research Center (ICRC) at the Petit Institute for Bioengineering and Bioscience.
The term “mutation” is typically used to encompass a broad spectrum on genomic level lesions ranging from small changes in the single letter DNA code (point mutations) to large chromosomal deletions and rearrangements (structural mutations) that can adversely affect the architecture and function of cells.
The explosion in the number of genome sequencing studies carried out over the past several years comparing normal and cancer tissues has generated an abundance of genome databases ripe for computational analyses of the spectrum of mutations associated with cancer.
In a study just reported in the online journal BMC Medical Genomics McDonald and Vinay Mittal (former graduate student in McDonald’s lab, now a bioinformatics scientist with Thermo Fisher Scientific in Michigan) report the results of a detailed analysis of structural mutations associated with ovarian cancer – the deadliest of all gynecological cancers.
Unlike most computational analyses of cancer mutations, the authors not only analyzed the structural variants found in cancer tissues but also those naturally occurring mutations present in the normal tissues of the same patients.
“The results were remarkable in the shear number of structural mutations identified,” says McDonald. They found 4,516 structural mutations in the cancer tissues and 5,518 in the normal tissues.
“Most of the structural variants identified are probably of little functional significance,” says Mittal. “But around 10 percent of the variants identified are ‘gene-fusions’ with the potential to generate hybrid proteins that may contribute significantly to cancer onset and progression.”
Disease of Misinformation
In addition to identifying and categorizing all of the structural variants associated with the ovarian cancer patients, Mittal and McDonald went on to determine the extent to which these variants were actually being expressed in the normal and cancer tissues.
While our DNA harbors all of the genetic information in our cells, like a blueprint, not all of this information is transmitted or “expressed” at any given time. Information in DNA must be transmitted to an intermediary RNA molecule before it can result in the manufacture of a functional protein. For example, many of the genes necessary for liver cell function are not expressed in the brain, and vice versa.
The detailed pattern of regulatory controls typical in normal cells is often disrupted in cancer cells. Thus, cancer cells not only contain DNA lesions or mutations not detected in normal cells, they may also display abnormal expression patterns, “genetic information that is silenced in normal cells but abnormally expressed in cancer cells,” says McDonald, who has called cancer, “a disease of misinformation.”
Cells get wrong information, such as being told to rapidly divide when they should be inactive. It could be an error in the cell’s blueprint (a mutation). Or, it could be an error in the flow of information (abnormal expression), a regulation problem, which gets to what may be the most remarkable and unexpected finding of the study, according to McDonald.
“At least some of the functionally significant abnormal gene-fusions expressed in the cancer tissues are also present in normal tissues,” he says. “But they are not being expressed.”
The results of the study underscore the importance of gene regulation in cancer. It raises questions about how and when cancer is due to a de novo mutational event or a mistake in information flow.
“The accumulation of structural variants and other mutations in our cells with the potential to cause cancer may be inevitable as we age, but our cells may naturally strive to suppress the expression of some of this misinformation,” says McDonald. “This suggests that while mutations may be necessary for the onset of most cancers, they my not be sufficient. We need to better understand the regulatory mechanisms that can suppress cancer causing mutations in some individuals and how these mechanisms break down in cancer patients.”
Studies are currently on-going to see if the suppression of cancer causing genetic lesions extends to other classes of mutation and to understand the molecular processes that may underlie the suppression mechanism. The hope is that this work will lead to novel and more effective therapies and treatments for cancer.
The Parker H. Petit Institute for Bioengineering and Bioscience, an internationally recognized hub of multidisciplinary research at the Georgia Institute of Technology, brings engineers, scientists, and clinicians together to solve some of the world’s most complex health challenges. With 17 research centers, more than 170 faculty members, and $24 million in state-of-the-art facilities, the Petit Institute is translating scientific discoveries into game-changing solutions to solve real-world problems.
CONTACT:
Jerry Grillo
Communications Officer II
Parker H. Petit Institute for
Bioengineering and Bioscience
<p><a href="http://hg.gatech.edu/node/jerry.grillo@ibb.gatech.edu">Jerry Grillo</a><br />Communications Officer II<br />Parker H. Petit Institute for<br />Bioengineering and Bioscience</p>
